“Acne” (acne vulgaris) is one of the most common skin conditions, affecting people of all ages. Many individuals first encounter Acne during puberty, but for some, its impact may extend well into adulthood.
Some women notice that their Acne worsens after stopping “the pill” (the combined oral contraceptive pill).
This is because some people’s oil glands are particularly sensitive to androgens (male sex hormones) which we all have! and produce more oil in response to these circulating hormones. The pill provides a lot of hormonal stabilisation, so when the pill is discontinued, the re-emergence of natural hormonal fluctuations, especially those involving androgens, may lead to increased sebum production and subsequent flare-ups.
In this guide, we explore the role of hormonal changes in “Post-Pill Acne” and introduce The Klira Special – a targeted skincare solution designed to address multiple facets of Acne.
Understanding Acne Vulgaris
What is Acne?
Acne vulgaris is a common skin condition characterized by a variety of lesions, including blackheads, whiteheads, papules, pustules, and in more severe cases, nodules or cysts.
Hormonal Acne is typically found on the lower face especially along the chin and jawline – but can appear anywhere on the face, neck, chest and back.
This occurs when the tiny oil-producing glands, known as sebaceous glands, become overactive and produce excess sebum, a natural oil that keeps the skin lubricated.
The underlying mechanisms of Acne
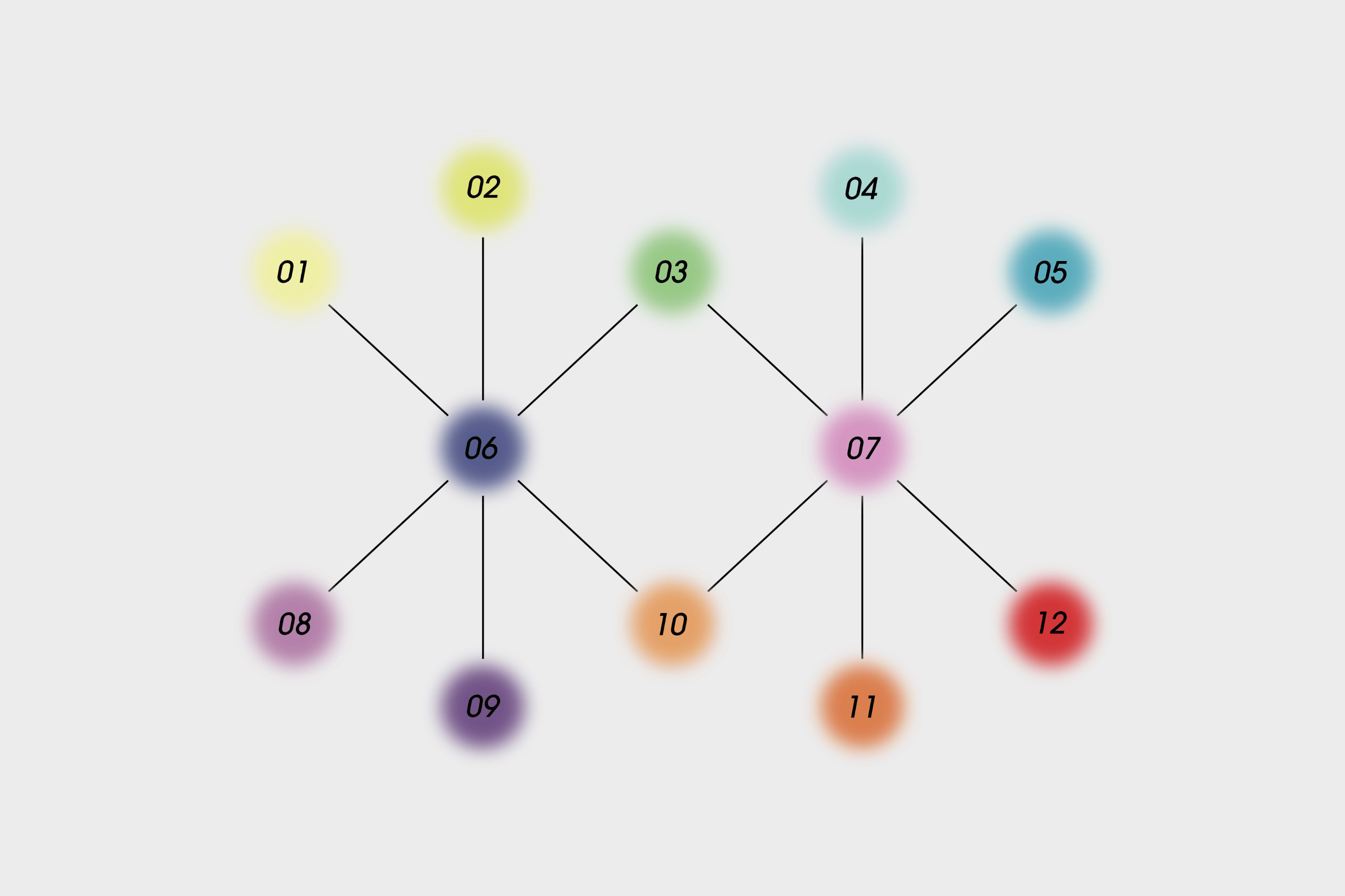
The development of Acne is a multifactorial process that involves several key elements:
- Excess sebum production: Hormonal influences, particularly androgens (male hormones that are also present in females), can cause sebaceous glands to produce too much oil. Some individuals have oil glands that are particularly sensitive to these androgens.
- Hyperkeratinisation: This is a process where the lining of the pore thickens due to an abnormal buildup of dead skin cells. This buildup can clog the pores, leading to the formation of blackheads and whiteheads.
- Bacterial colonisation: The clogged pore creates an ideal environment for bacteria – most notably Cutibacterium acnes – to multiply. Bacterial overgrowth can trigger an immune response, leading to inflammation.
- Inflammation: As the immune system reacts to the bacterial presence, inflammation occurs. This results in red, swollen, and sometimes painful lesions on the skin.
Together, these factors result in the various types of Acne lesions that many people experience. It is important to note that while acne can cause physical discomfort, it can also have a significant impact on mental health, affecting self-esteem and overall quality of life.
Hormonal influences in “Post-Pill Acne”
The role of hormones in Acne
Hormones play a central role in the development of Acne. Androgens, even at normal levels, can have a pronounced effect on the sebaceous glands in some individuals. When these glands are highly sensitive to androgens, they produce more sebum than is necessary, which, combined with the thickening of the pore lining, creates a breeding ground for bacteria and inflammation.
How “the pill” affects Acne
Combined oral contraceptive pills are often prescribed for reasons beyond birth control. One of their beneficial side effects for some women is the stabilisation of hormonal fluctuations.
By regulating hormone levels, the pill can help reduce the overactivity of sebaceous glands and subsequently, the severity of acne.
However, it’s important to understand that the pill’s primary use is not the treatment. Its use is generally reserved for those with a clear hormonal component to their acne, such as women whose breakouts are worse at specific times of the month, or those with polycystic ovary syndrome (PCOS).
What happens when you stop the pill?
When a woman discontinues the pill, the hormonal balance that was previously maintained begins to shift back to its natural state. For women with androgen-sensitive skin, this change can lead to an increase in sebum production, potentially triggering or exacerbating acne. This phenomenon is sometimes referred to as “post-pill acne,” although it is more accurately understood as a flare-up in response to hormonal rebound.
Strategies for managing Post-Pill Acne
Managing acne often requires a multi-pronged strategy. Traditional treatments include:
- Topical treatments: These are applied directly to the skin and include ingredients like benzoyl peroxide, topical antibiotics, and retinoids (such as tretinoin). They work by reducing bacterial load, unclogging pores, and promoting cell turnover.
- Oral medications: For more severe cases, oral antibiotics or hormonal treatments (including the pill or even anti-androgen medications like Spironolactone) may be prescribed.
- Isotretinoin: This is reserved for severe scarring. While highly effective, Isotretinoin comes with significant potential side effects and requires close monitoring.
Despite these options, many patients seek effective topical solutions that can be incorporated into their daily skincare routine.
Introducing The Klira Special
The Klira Special is a carefully formulated skincare treatment designed to address the multifaceted nature of acne vulgaris, especially in cases where hormonal changes – such as those following the discontinuation of the pill have triggered a flare-up. It combines several active ingredients, each chosen for its specific benefits in managing acne and promoting skin health.
The active ingredients and their benefits
- Tretinoin:
- Function: A derivative of vitamin A, tretinoin is well known for its ability to accelerate cell turnover. It helps to unclog pores by promoting the shedding of dead skin cells, thereby reducing the formation of blackheads and whiteheads.
- Benefit: By clearing blocked pores, tretinoin minimizes the risk of bacterial overgrowth and inflammation, which are central to acne development.
2. Azelaic Acid:
- Function: Azelaic acid possesses both antibacterial and anti-inflammatory properties. It helps to calm irritated skin and reduce the redness associated with lesions.
- Benefit: This ingredient not only combats the bacteria involved but also helps to even out skin tone, reducing the appearance of post-inflammatory hyperpigmentation (dark spots).
3. Aloe:
- Function: Renowned for its soothing and hydrating properties, aloe helps to alleviate irritation and maintain skin moisture.
- Benefit: By calming the skin, aloe minimizes the discomfort often associated with active treatments, making the overall regimen more tolerable.
4. Ivermectin:
- Function: Although more commonly recognised for its anti-parasitic properties, recent research suggests that Ivermectin can also play a role in reducing skin inflammation.
- Benefit: Its inclusion in The Klira Special helps to temper the inflammatory response that is characteristic of acne, contributing to clearer and calmer skin.
5. Lipid Blend (Cholesterol, Ceramides, and Free Fatty Acids in a 1-2-1 Ratio):
- Function: This unique combination is designed to mimic the natural lipids found in the skin. Ceramides and free fatty acids help to repair and reinforce the skin’s barrier, while cholesterol plays a critical role in maintaining barrier integrity.
- Benefit: A healthy skin barrier is essential for preventing moisture loss and protecting the skin from external irritants. Restoring this barrier not only aids in healing but also reduces the likelihood of further irritation and inflammation.
How The Klira Special addresses Post-Pill Acne
Given the complex nature of Acne Vulgaris, particularly when exacerbated by hormonal changes, The Klira Special offers a comprehensive approach:
Exfoliation and pore clearance: Tretinoin helps to gently exfoliate the skin, reducing the buildup of dead skin cells that can clog pores.
Anti-inflammatory action: Azelaic acid and Ivermectin work together to control the inflammatory response, reducing redness and swelling.
Soothing and hydration: Aloe provides a cooling effect that calms irritated skin, while the lipid blend restores and maintains the skin’s protective barrier.
Overall skin health: By addressing multiple aspects of acne pathophysiology – from excess sebum production and clogged pores to inflammation and barrier dysfunction – The Klira Special helps to reduce the frequency and severity of breakouts that may occur after stopping the pill.
Self-care and additional considerations
Lifestyle and skincare practices
While topical treatments like The Klira Special can be highly effective, managing acne also involves good self-care and lifestyle practices:
Gentle cleansing: Use a mild, non-comedogenic (non-clogging) cleanser to remove dirt, oil, and makeup without stripping your skin of its natural moisture.
Sun protection: Many active ingredients, including Tretinoin, can increase your skin’s sensitivity to sunlight. Apply a broad-spectrum sunscreen daily to protect your skin from harmful UV rays.
Avoid picking: It may be tempting to pick or squeeze lesions, but this can worsen inflammation and lead to scarring. Instead, allow your skin to heal naturally. There are plenty of soothing hydrocolloid plasters on the market which you can apply last thing at night to stop compulsive picking!
Diet and hydration: While there is limited evidence linking specific diets to acne, a well-balanced diet and proper hydration support overall skin health.
Emotional well-being: Acne can have a significant impact on self-esteem and mental health. If you find that your skin condition is affecting your mood, consider speaking with a healthcare professional or counselor for additional support.
When to consult a healthcare professional
If you notice that your acne worsens significantly after stopping the pill or if over-the-counter treatments are not providing sufficient improvement, it is important to consult a healthcare professional such as a Dermatologist. They can help determine whether your acne is primarily driven by hormonal factors, guide you on the appropriate treatment regimen, and monitor for any side effects.
In cases of severe or persistent acne, a dermatologist may recommend additional treatments such as oral antibiotics, Isotretinoin, or even hormonal therapies like Spironolactone.
In Summary
Acne vulgaris is a complex skin condition influenced by a combination of genetic, hormonal, and environmental factors. For women who have experienced improvement while taking the combined oral contraceptive pill, discontinuation can sometimes lead to a rebound in acne – especially if their oil glands are sensitive to androgens.
Understanding the underlying mechanisms of acne, including excess sebum production, follicular blockage, bacterial overgrowth, and inflammation, is essential for effectively managing this condition.
The Klira Special offers a modern, multifaceted approach to addressing post-pill acne by combining powerful active ingredients such as Tretinoin, Azelaic Acid, Aloe Vera, Ivermectin, and a restorative lipid blend. This formulation not only works to unclog pores and reduce inflammation but also soothes and repairs the skin’s natural barrier, paving the way for clearer, healthier skin.
By incorporating both effective topical treatments and sound self-care practices, individuals can better manage the transition following pill discontinuation and reduce the impact of acne vulgaris on their lives.
Remember that every skin is unique; what works for one person may not work for another. Therefore, a personalised approach – ideally designed by a Dermatologist – is the best strategy for achieving long-term improvement.
For further reading on post-pill acne, visit The British Association of Dermatologists and to learn more about The Klira Special and its ingredient breakdown, check out The Klira Special page.
This guide is intended for informational purposes and should not replace professional medical advice. Always consult your healthcare provider to determine the most appropriate treatment for your individual skin needs.
Our Dermatology Team will review your SkinSize™ Analysis, medical information, and photos to decide which ingredients you will receive in your bespoke formula.